Oral candidiasis (oral thrush)
Newborn infants, those with HIV infection or having chemotherapy or radiotherapy for cancer, asthmatic patients using inhaled steroids or antibiotics are most susceptible to oral thrush. Oral thrush appears as curdy, white patches or membranes covering the inside of the mouth or on the tongue. The mouth feels coated and uncomfortable. Under the white patches the mucosa is reddened and irritated. Some of those affected just have red areas without a white membrane. Oral thrush responds well to treatment which is usually topical nystatin, miconazole, amphotericin B or fluconazole capsules. Most instances are due to Candida albicans – occasionally other species and sometimes it is fluconazole resistant, especially if it has already been treated multiple times. More info
Vaginal candidiasis (vaginal thrush or yeast infection)
Up to three quarters of all women will suffer at least one episode of vaginal thrush during their lifetime. The precise factors are unknown, but vaginal candidiasis is associated with pregnancy, diabetes and antibiotic treatment, but no HIV infection (unlike oral thrush). Most of these women experience infrequent attacks and respond well to drug therapy; however in some the infection is recurrent or persistent or responds less well to drug therapy. It is estimated that ~135 million women suffer recurrent episodes of vaginal thrush in any given year and this problem can be present for a couple of years of much longer, for poorly understood reasons.
Symptoms of thrush include vaginal discharge, intense vaginal and vulval itching (pruritis), painful or difficult urination (dysuria) and difficult or painful sexual intercourse (dyspareunia). In women who are not pregnant infection tends to begin the week before menstruation. Thrush is so common that often a woman can obtain treatment from a doctor without a genital examination. Many other conditions mimic vaginal candidiasis especially bacterial vaginosis and various forms of eczema-like conditions. If symptoms persist despite antifungal treatment it is necessary to perform a genital examination and obtain specimens for laboratory diagnosis and check for other conditions. This allows the doctor to eliminate other causes of disease such as bacterial infection and to test for drug resistance in any Candida yeasts isolated. More info
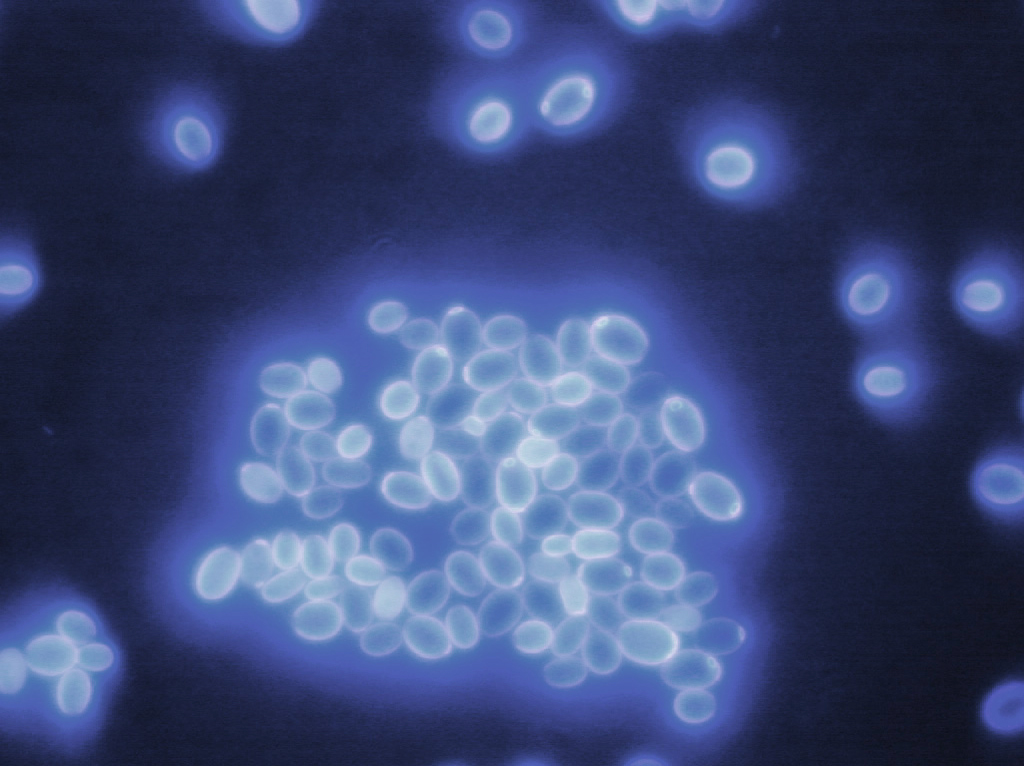
About 95% of vaginal candidiasis is caused by the yeast Candida albicans with a further 5% caused by Candida glabrata; infections with Candida glabrata tend to be milder, but unresponsive to fluconazole or clotrimazole Candida albicans has been isolated from vaginal swabs in women who do not complain of symptoms and who do not have clinical signs of disease. This suggests that some change in the vaginal environment needs to occur for the yeast to cause disease.
Most women with thrush respond to topical treatment with the antifungal drug nystatin or an antifungal drug from the imidazole family – clotrimazole, econazole, isoconazole or miconazole. Clotrimazole, econazole and miconazole are sold as creams and clotrimazole, econazole, isoconazole and miconazole are sold as pessaries. The imidazole drugs have a higher cure rate than nystatin with shorter courses of treatment. Two other drugs, itraconazole and fluconazole are available in an oral form for the treatment of thrush. Fluconazole is given in a single oral dose and itraconazole in two doses 8 hours apart. Fluconazole and itraconazole are more expensive than the other drugs, but are easier and less painful to administer. Fluconazole and itraconazole should not be given if there is any chance of pregnancy.
Women with recurrent thrush may suffer from depression and psychosexual problems and it is important to obtain a cure as quickly as possible. It is often helpful for the patient to think of factors that may trigger the infection. It is also important for a patient to consider that their sexual partner may be colonised with Candida yeasts (this can occur without symptoms) and may pass the infection on to them during sexual intercourse. It is not necessary to investigate oral or intestinal colonisation with Candida yeasts. In the past doctors thought women had recurrent vaginal thrush because they were reinoculated from a persistent intestinal reservoir; this is now known to be false.
Recurrent vaginal candidiasis can be controlled in most women using longer term treatment with oral antifungals. After symptoms of thrush have been suppressed for six months, drug treatments are discontinued and the patient is reassessed. Many women do not revert to the previous pattern of recurrent disease. Some women find that yoghourt douches or special diets help them. It is also recommended that women with recurrent thrush wear loose fitting cotton underwear and do not wear tights.
Penile candidiasis (penile thrush, Candida balanitis)
Most men with penile candidiasis experience an inflamed penis apex and foreskin and sometimes they have a discharge from underneath the foreskin. The apex of the penis is often red with spots and the skin on the penis and in the groin is sometimes itchy and scaly. A specimen will often be taken for laboratory diagnosis as these symptoms can result from other infections. Penile candidiasis is treated with saline washes or application of antifungal cream. Female partners should be examined in case they are the source of the infection. If a man has a persistent infection, he should be investigated for diabetes as diabetes sufferers are prone to penile candidiasis. In addition men who have a penile catheter inserted for a long time are prone to recurrent penile candidiasis. More info
Chronic mucocutaneous candidiasis (CMC)
CMC is a rare condition caused by the yeast Candida. Most people can fight off Candida infections with the use of antifungal treatment, but in a small number of people these infections recur and are difficult to cure. It is a usually genetic disorder with several different genetic causes. Occasionally there are other reasons for recurrent thrush and blood tests are needed to eliminate these. In CMC, individuals have frequent, usually continuous oral thrush which can be difficult to treat. Most cases of CMC are recognised in childhood where babies or children have repeated episodes of oral thrush and sometimes thrush of the gullet (oesophagus).
In genetic forms of CMC other health problems occur with increasing age. The immune systems of these people, although unable to fight off Candida, are overactive in certain body tissues. Damage to endocrine organs like the adrenal glands and ovaries and also to the skin can occur in adolescence or early adulthood. Some patients develop patches on their skin (vitiligo) and others lose some or all of their hair.
Although most cases of CMC occur in childhood, there are some cases that first appear in adults even as late as 50 years of age. These cases are not so clearly linked to a genetic defect and the cause(s) of CMC in adults is unknown. People who develop CMC as adults are unlikely to experience the additional problems that people who develop CMC as children can experience.
CMC is usually treated with long courses of oral antifungals such as fluconazole or itraconazole. These drugs have a side effects and long term therapy, even for many years at a time, appears safe. A slight concern is that antifungal drug resistance may occur over time.
Deep Candida infections
Oesophageal candidiasis
People with HIV infection or who are unwell with other severe illnesses can develop Candida infection of the oesophagus. In mild cases it can be asymptomatic, but in more severe cases can leading to nausea, vomiting, difficulty swallowing and discomfort in the centre of the chest. It is often difficult to diagnose based on symptoms alone and endoscopy (looking at the oesophagus with a fibre optic scope) is required. Most cases are caused by the yeast Candida albicans with a few by Candida glabrata. Treatment with fluconazole for 10-14 days usually resolves the infection; if not then itraconazole solution or intravenous echinocandin or amphotericin B are almost always effective. More info
Candida bloodstream infection (candidaemia)
Candida may enter the bloodstream and lead to disseminated disease, otherwise known as invasive candidiasis. Patients ar risk include critically ill patients in intensive care, especially those with diabetes or renal failure. It is linked to the number of antibiotics given and also immune suppression. Some patients have had gastrointestinal, pancreatic, transplant or thoracic surgery or they are receiving nutrition intravenously. Extremely premature babies are also at high risk but otherwise rates of Candida bloodstream infection rise with age. About 35% of those with Candida bloodstream infection are extremely unwell with septic shock.
The commonest clinical features are fever, increased shortness of breath or oxygen requirement and increasing inflammatory markers in the blood. Rash is unusual, unless caused by Candida tropicalis. These features are very similar to bacterial sepsis and often antibiotics are given without antifungals. Blood cultures are positive in about 40% of patients with invasive candidiasis; some patients have silent dissemination and then end up with focal features of disseminated candidiasis including a heart valve, bone or internal eye infection. More info
About 50% of these infections are caused by the yeast Candida albicans, although other Candida yeasts are also implicated, these including Candida glabrata, Candida parapsilosis, Candida tropicalis and recently Candida auris. Accurate diagnosis of the Candida yeast species is important because different species have different susceptibilities to antifungal drugs.
The current best therapy for most people with Candida bloodstream infection is one of the echinocandins (caspofungin, anidulafungin or micafungin) Amphotericin B and fluconazole and the main alternatives Amphotericin B is also available in safer lipid formulations. Flucytosine is occasionally used for resistant Candida species or if eye or urine infection is found, because it is water soluble and gets to the site of infection, as does fluconazole and unlike echinocandins.
Candida auris is an emerging pathogen, first reported in 2009 from an ear canal infection in Japan. It is associated with life-threatening invasive diseases such as bloodstream and wound infections globally. In a span of only seven years, this yeast has become widespread in several countries, It is able to colonise the skin, especially the groin and armit, invade and cause disease with varying severity in different people. More Info
Globally about 626,000 people each year grow Candida in their bloodstream, which is a very serious infection and leads to about 254,000 deaths. Probably another 939,000 have silent dissemination of Candida in their body, also with life-threatening consequences (an estimated 742,000 deaths).

Candida peritonitis (intra-abdominal candidiasis)
After bowel surgery, some people get infection inside their abdomen. Such infections are often mixed bacterial and Candida infections. It is important that Candida is treated with antifungals in these patients as antibacterials alone are insufficient. More info

