Aspergillus
Aspergillus is a type of mould which is found everywhere in the air and soil world-wide, especially in the autumn and winter in the Northern hemisphere. Only a few of these types of moulds can cause illness in humans and animals. Most people are naturally immune and do not develop disease caused by Aspergillus. However, when disease does occur, it takes several forms.
The type of diseases caused by Aspergillus are varied, ranging from an “allergy”-type illness to life-threatening generalised infections. Diseases caused by Aspergillus are called aspergillosis. The severity of aspergillosis is determined by various factors but one of the most important is the state of the immune system of the person.
Chronic Pulmonary Aspergillosis (CPA)
CPA is a slowly progressive destructive disease of the lung, leading to loss of respiratory function, and general ill health (weight loss, coughing, bringing up blood, shortness of breath). It is almost always caused by Aspergillus fumigatus. Underlying diseases include tuberculosis, atypical tuberculosis, chronic obstructive pulmonary disease (COPD, emphysema), pneumothorax, sarcoidosis, allergic bronchopulmonary aspergillosis, lung cancer treatment. Without adequate treatment ~50% of patients die in 5 years, often by coughing up large quantities of blood. There are estimated to be 2000-3000 people in the UK living with this condition, but over 1.8 million new people worldwide. It is thought that this leads to about 340,000 deaths each year, many mis-diagnosed as having pulmonary tuberculosis.
Aspergilloma
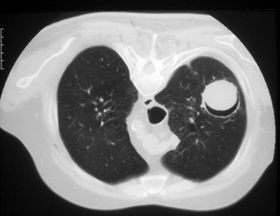
This is a very different disease also caused by the Aspergillus mould. The fungus grows within a cavity of the lung, which was previously damaged during an illness such as tuberculosis or sarcoidosis. Any lung disease which causes cavities can leave a person vulnerable to developing an aspergilloma. The spores penetrate the cavity and germinate, forming a fungal ball within the cavity. The fungus secretes toxic and allergic products which may make the person feel ill. More info
The person affected may have no symptoms (especially early on). But weight loss, a chronic cough and feeling rundown are common symptoms later. Coughing of blood (haemoptysis) can occur in up to 50-80% of affected people.
The diagnosis is made by X-rays, scans of lungs and blood tests.
Treatment depends on many factors including whether the patient is coughing blood and how much lung disease there is. Oral itraconazole (usually 400 mg daily) helps symptoms in many patients but rarely kills the fungus in the cavity. Sometimes surgical removal is possible, especially if the patient is coughing blood. Sometimes other antifungal drugs (especially amphotericin B) can be injected directly into the cavity by a tube which is put into position under local anaesthesia. Up to 10% of cases get better without treatment, especially if there are no symptoms.
Allergic bronchopulmonary aspergillosis (ABPA)
This is an allergic fungal disease affecting asthmatics and cystic fibrosis patients. Patients cough up thick plugs of mucus, and are short of breath and tired. Over years, the airways become thickened and wider (bronchiectasis), and multiple bacterial infections are common. It may evolve into CPA. Antifungal treatment has a major impact on quality of life in most patients, particularly in improve breathing and energy levels. Some of these patients also have serious nasal disease. ABPA affects ~1% of adult asthmatics (~40,000 people) and about 15-25% of adult cystic fibrosis patients (~300-500 people). More info.
Severe Asthma with Fungal Sensitisation (SAFS)
Severe asthmatics may be sensitised (allergic) to multiple fungi, and this disease is called Severe Asthma with Fungal Sensitisation (SAFS). Aspergillus is the commonest fungus to which they are sensitized. Those affected have multiple exacerbations of asthma requiring steroids and antibiotics many times a year, being admitted to hospital and generally suffering a poor quality of life. Antifungal therapy helps most of these patients. In the UK there are estimated to be 190,000 – 300,000 affected. More info.
Aspergillus sinusitis
Aspergillus disease can happen in the sinuses leading to Aspergillus sinusitis. This happens in a similar way to aspergilloma. In those with normal immune systems, stuffiness of the nose, chronic headache or discomfort in the face is common. Drainage of the sinus, by surgery, usually cures the problem, unless the Aspergillus has entered the sinuses deep inside the skull. Then antifungal drugs and surgery is usually successful.
When patients have damaged immune systems – if, for example they have had leukaemia or have had a bone marrow transplant-Aspergillus sinusitis is more serious. In these cases the sinusitis is a form of invasive aspergillosis (see below). The symptoms include fever, facial pain, nasal discharge and headaches. The diagnosis is made by finding the fungus in fluid or tissue from the sinuses and with scans. Treatment with powerful antifungal medicines is essential (e.g. amphotericin). Surgery is done in most cases as it is important to find out what is exactly wrong and is often helpful in eradicating the fungus. More info.
Chronic rhinosinusitis is often caused by fungi, of which Aspergillus is the most common in the UK (fungal rhinosinusitis). Those affected have blocked noses, loss of smell, continuous discharge from their nose, recurrent sinus infections and usually nasal polyps. It is a long-term condition requiring endoscopic or open surgery, and usually relapses after surgery. Local steroid sprays and treatment of bacterial sinusitis is the main treatment, as antifungal therapy is not always effective (and not convincingly demonstrated to be useful). Chronic rhinosinusitis affects 18% of the UK young adult population (and fungi play a role in 7%), so fungal rhinosinusitis is estimated to affect ~400,000 people in the UK.
Invasive aspergillosis

Many people with damaged or impaired immune system die from invasive aspergillosis. Their chances of living are improved the earlier the diagnosis is made but unfortunately there is no good diagnostic test. Often treatment has to be started when the condition is only suspected.
This condition is usually clinically diagnosed in a person with low defences such as bone marrow transplant, low white cells after cancer treatment, AIDS or major burns. There is also a rare inherited condition that gives people low immunity (chronic granulomatous disease) which puts affected people at moderate risk. People with invasive aspergillosis usually have a fever and symptoms from the lungs (cough, chest pain or discomfort or breathlessness) which do not respond to standard antibiotics. X-rays and scans are usually abnormal and help to localise the disease. Bronchoscopy (inspection of the inside of the lung with a small tube inserted via the nose) is often used to help to confirm the diagnosis. More info.
Sometimes the fungus can transfer from the lung through the blood stream to the brain and to other organs, including the eye, the heart, the kidneys and the skin. Usually this is a bad sign as the condition is more severe and the person sicker with higher risk of death. However, sometimes infection of the skin enables the diagnosis to be made earlier and treatment to be started sooner.
Treatment is with antifungal drugs such as amphotericin B and/or itraconazole. Amphotericin B has to be given by vein in large doses. In some patients the treatment can damage kidney and other organs. Newer forms of amphotericin B (Amphotec or Amphocil, Abelcet or AmBisome) are useful, especially when the patient experiences side-effects, as there are less toxic. Itraconazole is generally given orally (also in large doses, e.g. at least 400 mg daily). The earlier treatment is started the better the chances of survival. In patients with low numbers of white cells (infection fighters), recovery of these cells can be important in stopping the growth of the fungus. Sometimes surgery is also required. Overall, about a third of patients survive invasive aspergillosis if treated and none survive if they are not treated.
All these conditions can affect children and should be diagnosed and treated in the same way.
A lot of encouraging research is being done at the moment to speed up diagnosis of this invasive aspergillosis and to improve its treatment. Some new antifungal drugs are in clinical trials at present.
A 2024 global estimate of the number of people affected by invasive aspergillosis is 2,113,000 people as a secondary infection of chronic obstructive pulmonary disease (COPD, or smoke-related lung disease), intensive care, lung cancer or leukaemia. Of these 1,801,000 (85·2%) are thought to die, partly because the diagnosis is not made or is too late.
